Supporting Commercially Insured Members with Kidney Disease: Lessons from the Field
Author : Sarah Katz, National VP, Payor PartnershipsKidney disease on the rise in the under 65 population
Although kidney disease is often viewed as a disease of the elderly, prevalence in the under 65 population is substantial and on the rise, increasing from 7.8% in 2010 to 8.8% in 2019, an overall increase of 13%. With COVID’s impact on preventive care and screenings still playing out, this number is unfortunately likely to increase further.
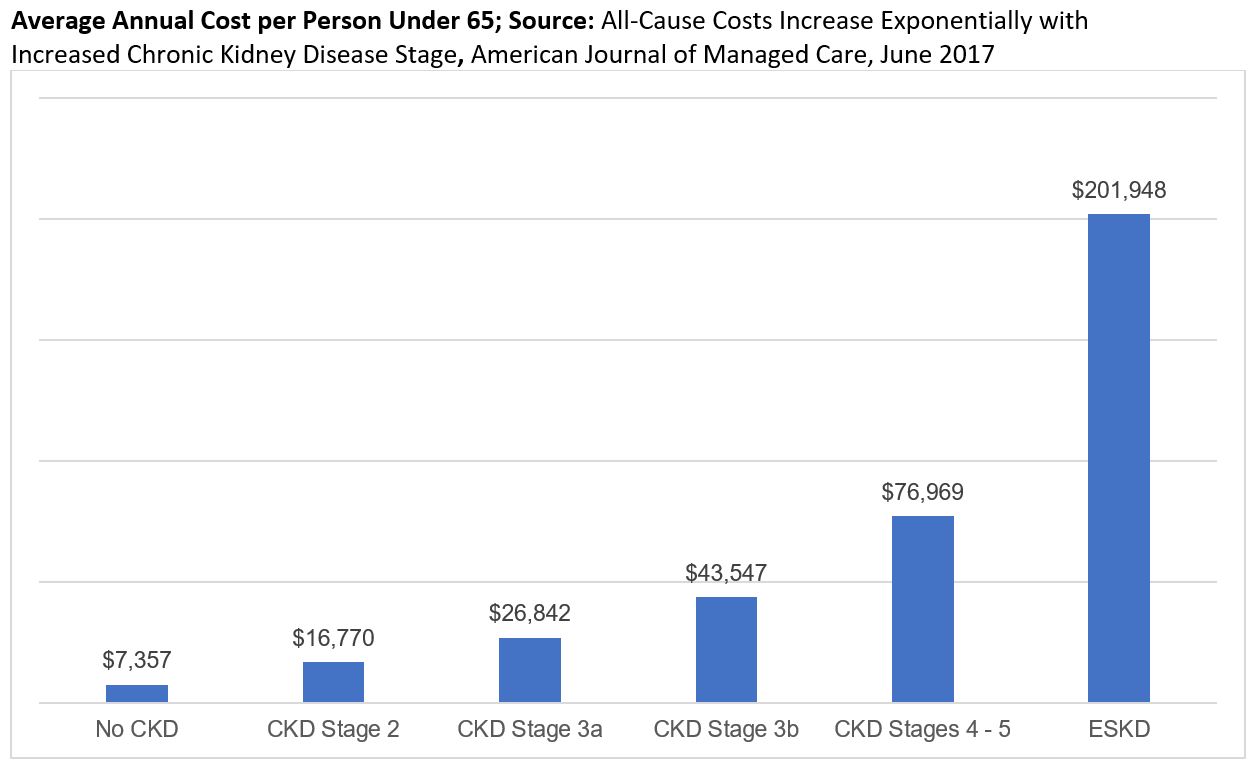
The impact of this high prevalence rate is compounded by the significantly higher cost of care for individuals with chronic kidney disease (CKD) and end-stage kidney disease (ESKD). The weighted average per member per month (PMPM) cost for individuals under 65 with advanced kidney disease (CKD 4 through ESKD) is $8,300 — compared to $600 for individuals who do not have kidney disease.
As a result, employers — who have traditionally focused on offering disease management for diabetes and heart disease — are turning their attention to kidney care and learning that care for these complex patients requires a more comprehensive approach than a traditional disease management solution. Beyond the cost implications, the profound, negative impact CKD and ESKD has on quality of life is of great concern to employers.
Inpatient utilization primary cost driver for commercially insured
An analysis by the American Journal of Managed Care found that for commercially insured members, costs increase by 98% with each disease stage. For patients with CKD, these increases are primarily driven by hospitalizations, which account for 60% of the total cost of care, followed by outpatient care, pharmaceuticals and ED visits. Inpatient spend is even the primary cost driver for patients with ESKD, for whom dialysis is typically thought of as the highest area of cost (dialysis ranks second).
Unlocking Success in the ACO REACH Program Through Kidney Disease Management
Read NextNumerous points of evidence suggest that disease progression, and by extension a significant portion of hospitalizations, is preventable through effective and timely care. Over 30% of CKD and ESKD admissions were readmissions, the vast majority of which are potentially avoidable. Strive’s care model has achieved up to a 40% reduction in all admissions with our partners and a 10% 30-day readmission rate (compared to the national average of 22.3% for patients with kidney disease).
Taken together, this evidence indicates that a focus on slowing disease progression—and by extension reducing associated hospitalizations and readmissions—through proactive, comprehensive kidney care, substantially reduces total cost of care while improving quality of life.
Four key program elements to support individuals with kidney disease
In light of these trends, employers are beginning to explore options to support their employees and dependents with kidney disease. Since this is a relatively new space—particularly in comparison to more established disease management efforts for diabetes and heart failure—many are unsure which interventions will be most valuable and move the dial on the cost of care.
Within this new and evolving field, Strive Health’s success managing commercially insured populations—achieving ~$900 PMPM savings for all admissible members—has revealed four program elements critical to success.
Element #1: Advanced predictive analytics to identify all individuals at high risk of progression
Among patients with early-stage CKD (Stages 1-3), a subset is at risk for rapid progression to ESKD and should be prioritized for engagement. Unfortunately, since over half of early-stage CKD is undiagnosed, there’s rarely sufficient data to fully identify this population. Recognizing this critical gap, Strive has developed advanced models to close data gaps and predict risk of progression to ESKD—for all individuals—with 93% accuracy. This approach significantly expands the scope of impact for preventive care efforts.
Element #2: High-touch care model
For individuals with CKD, adherence to an established care plan and regular labs to monitor disease status are essential to prevent disease progression. In the current state of kidney care, most CKD patients are treated by a primary care provider (PCP) who has limited resources to proactively monitor care plan adherence. In Strive’s experience, having a dedicated, in-market specialized kidney care team that monitors patient engagement and proactively follows up when patients disengage overcomes this gap. The care management team works in full coordination with the PCP (or other providers) to ensure consistent and efficient messaging to each patient.
Such teams must be flexible to meet with patients however is easiest for them (in-home, virtual or in-clinic) and have same-day, same-hour availability so they can help patients manage symptom escalation, avoid costly ER visits, admissions, and ultimately prevent disease progression.
Element #3: Holistic condition management
Individuals with CKD and ESKD are highly likely to have other chronic illnesses, most frequently hypertension (89% of CKD patients) and diabetes (38% of CKD patients). Since managing just one chronic illness can take a significant amount of time and energy, individuals with CKD in addition to other chronic diseases need to be supported with a comprehensive solution that can address all their health needs. In Strive’s experience, incorporating condition management-specific programs that all team members are trained on has allowed us to serve as a one-stop resource. By taking this approach, 80% of Strive enrollees with diabetes have their blood sugar controlled and 93% of enrollees with hypertension have their blood pressure controlled.
Element #4: Local provider coordination
Finally, an effective kidney care solution program cannot operate in a vacuum. Most individuals likely already have a preferred PCP or nephrologist, and a comprehensive kidney care solution should support that provider in delivering care. Failure to do this will result in patient and provider abrasion and limit the success of the program. An on-the-ground provider integration team—to supplement the core care management team—can establish communication preferences and ensure the patient has a coordinated experience once enrolled. Strive deploys a Provider Integration team in all markets that collaborates practice to practice to develop relationships, share how Strive can support providers and their patients and define workflow/communication standards.
Learn how Strive is improving outcomes and reducing the cost of care for commercially insured populations
By incorporating these elements into our comprehensive kidney care model, Strive has delivered significant value to commercially insured populations, achieving up to $900 PMPM savings for all members.
To learn more about our approach and how we can support your plan members with kidney disease, please connect with us here.