Unlocking Success in the ACO REACH Program Through Kidney Disease Management
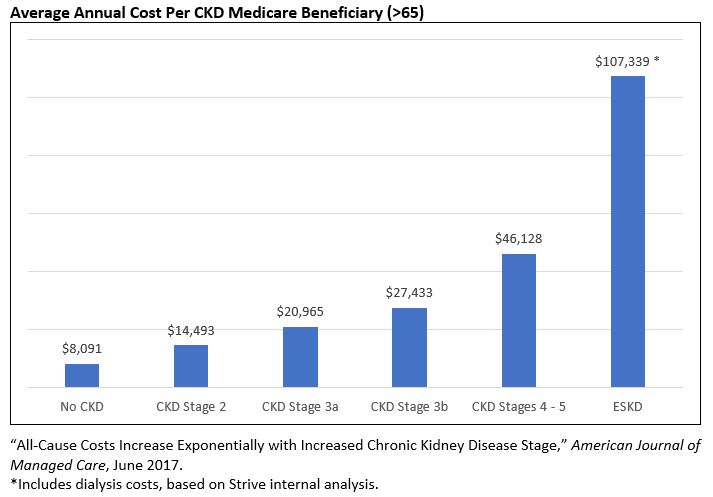
Author : Sarah Katz, National VP, Payor PartnershipsWith the 2023 performance year now underway, the 110 provisionally accepted CMS REACH ACOs are analyzing their attributed population to prioritize clinical initiatives. While evergreen high-cost areas such as diabetes, hypertension and cardiovascular disease are sure to top the list, kidney disease is an often-overlooked target—due to being asymptomatic in earlier stages—that drives costs directly and exacerbates other chronic conditions, indirectly increasing total cost of care. In 2019, care for Medicare beneficiaries with chronic kidney disease (CKD) cost the U.S. $87.2 billion, and those with end-stage kidney disease (ESKD) cost an additional $37.3 billion. Given this interrelated dynamic, a successful kidney disease management strategy can determine ACO success.
Kidney disease a key cost driver for ACOs due to challenges in diagnosis and treatment
With a 38% prevalence rate in >65 population and a 48% increase in costs as patients advance a single disease stage, chronic kidney disease (CKD) management is a critical competency for ACOs. Since CKD is largely asymptomatic until stage 4 / 5 (90% of individuals are unaware they even have it), proactive testing is key to preventative management. However, available data and anecdotal evidence suggest there is significant room for improvement in testing among primary care physicians (PCPs).
A recent study found that PCPs only completed comprehensive, annual testing for CKD in 51.6% of patients with type 2 diabetes (note the study used data from 2016-2019, so care avoidance due to the pandemic was not a factor). This is despite diabetes being one of the most common causes of CKD and 40% of diabetics having a confirmed CKD diagnosis.
More advanced practices may perform better on testing but still face challenges in managing patients with CKD once diagnosed. Medications may be able to support CKD management depending on the cause of disease, but lifestyle changes (diet, exercise, smoking cessation) are central to prevent progression.
Strive’s experience has demonstrated that repeated, extensive interactions with kidney specialized care team members are critical to support patients in achieving sustainable lifestyle changes that prevent disease progression. CKD is highly complex—particularly regarding dietary implications—and patients need specialized, on-demand support to address any questions on their care plan.
Given short appointment times and competing concerns to address, it is almost impossible for PCPs to directly deliver education on this complex topic. While many practices—particularly those participating in an ACO—have multidisciplinary care teams supporting the PCP, these teams often have high panel sizes and lack the kidney-specific expertise required to support the CKD population effectively.
ESKD performance challenged by benchmark methodology and nephrologist alignment
While patients with ESKD comprise only ~1% of the Medicare population, they can have an outsized impact on ACO performance given their high cost (over $100,00 per person with dialysis costs included). Aside from the general challenges of managing a complex population, there are two challenges specific to managing ESKD patients in ACO REACH (or other CMS-sponsored ACO programs):
- Benchmarks for the ESKD population are based on an ACO’s historical expenditure and the ACO REACH Rate Book. The Rate Book uses state-level data to determine a benchmark rate and may not reflect the high costs of a given market, putting ACOs at substantial risk. This is especially problematic for new entrant ACOs whose benchmarks are based entirely on the Rate Book and not historical expenditures.
- Lack of network control means ACO beneficiaries are able to see any Medicare participating provider, creating substantial risk if patients see a low-value nephrologist and/or one with whom they do not have a strong working relationship. This limits the ability to coordinate care, particularly around renal replacement therapy planning. Having a strong PCP–nephrologist–patient connection during the planning phase substantially increases the likelihood of patients opting for home dialysis, which is significantly less expensive than in-center, provides superior quality of life and often improves clinical outcomes.
Three priority capabilities to support patients with CKD and ESKD
Long-term success in managing a kidney disease population requires a comprehensive set of specialized capabilities ranging from risk stratification to performance evaluation. Given the short timeframe until the ACO REACH program launches, Strive recommends ACOs prioritize three capabilities for initial rollout while pursuing a broader solution.
- Advanced predictive analytics to identify undiagnosed CKD: Typically part of a broader risk stratification platform, specialized machine-learning algorithms can flag patients at high risk for CKD. To increase predictive accuracy, algorithms should incorporate factors beyond common comorbidities such as genetic predisposition, lifestyle and socioeconomic factors. More sophisticated platforms will then automatically prompt the patient’s provider to engage the patient and order comprehensive testing.
- Specialized, in-market kidney care management team: CKD and ESKD are highly complex conditions that often require significant lifestyle changes. To effectively support patients in making these changes, Strive deploys an in-market, multidisciplinary Kidney Hero™ team that utilizes motivational interviewing to help patients craft personalized, achievable care plans. Low panel sizes allow team members to spend upwards of an hour with a patient on an ongoing basis, which is highly effective for patient education given the complexity of CKD and ESKD. In addition, this enables our team to build trusting, long-term relationships that position us well to drive care plan adherence.
- Aligned nephrologist relationships: ACOs that do not currently have a preferred nephrologist partner should quickly determine which practices are most open to collaboration and how that aligns with current referral patterns and patient preferences. Longer term, ACOs may wish to engage nephrologists as preferred providers. This enables ACOs to create value-based arrangements with nephrologists that would tie shared savings payouts to adherence to workflow and communication standards and/or outcomes.
Learn how Strive works with ACOs
Strive has extensive experience working with Medicare ACOs and has achieved 20% total cost of care reduction for our partners. Our collaborative, provider-centric orientation ensures that we integrate seamlessly with existing workflows and deliver results while supporting patient and provider satisfaction. To learn more about our approach and how we can deliver results for your organization, please click here.